Depression is one of those words we hear all the time, but few people truly understand what it means. It’s often confused with sadness, burnout, or just “having a rough week.” But real depression: the kind that changes how you think, feel, and function, is far more complex.
If you’ve ever woken up feeling like the world has lost its color, like you’re walking through fog, or like everything takes ten times more effort than it should, you’re not alone. Millions of people experience this every year, and yet many still feel isolated or misunderstood.
Let’s talk about what depression really is, why it happens, and what can help you start feeling better again.
Disclaimer: This article is for informational and educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your doctor or a qualified mental health professional with any questions you may have regarding your health or a medical condition. If you are in crisis, please contact your local emergency services or a suicide helpline immediately.
What Is Depression?
Depression (also called major depressive disorder) is a medical condition that affects your mood, thoughts, energy, and ability to function day to day. It’s not just feeling sad; it’s a deep, persistent state of low mood that doesn’t simply “go away” with rest or positive thinking.
The World Health Organization estimates that over 280 million people worldwide live with depression at any given time.[1] That’s roughly one in every 20 adults.
While everyone feels down sometimes, depression is different because it lingers for weeks, months, or even years and it affects how you experience everything.
The Many Faces of Depression
Depression doesn’t look the same for everyone. There are several types, each with slightly different patterns and triggers:
- Major Depressive Disorder (MDD): The most common form. Marked by long periods of deep sadness, loss of interest, and changes in sleep or appetite.
- Persistent Depressive Disorder (Dysthymia): A milder but longer-lasting form that can last for years. People often describe it as “functioning, but numb.”
- Seasonal Affective Disorder (SAD): Depression linked to seasonal changes, often appearing in the darker months due to reduced sunlight exposure.
- Postpartum Depression: Occurs after childbirth, affecting both emotional and physical well-being. It’s far more than “baby blues.”
- Bipolar Depression: A type of depression that alternates with periods of high energy or mania.
- Atypical Depression: Characterized by mood improvement in response to positive events, along with symptoms like increased appetite or sleep.
Recognizing which type you’re experiencing can help guide treatment, but even if you’re unsure, know that any form of persistent low mood deserves attention and care.
How Depression Affects the Brain and Body
Depression isn’t “just in your head”. It’s also in your body and your brain chemistry.
Research shows that depression can change how certain parts of the brain function, especially those involved in emotion and motivation. The amygdala, hippocampus, and prefrontal cortex all play roles in regulating mood, decision-making, and stress response.[2]
In depression:
- The amygdala (linked to fear and emotion) becomes overactive.
- The prefrontal cortex (responsible for reasoning and control) becomes less active.
- The hippocampus (memory and mood regulation) can actually shrink with long-term depression.[3]
This combination leads to a brain that reacts more strongly to negative emotions and struggles to regulate them.
Physically, depression can affect your sleep, appetite, digestion, and energy levels. It’s also connected to increased inflammation and changes in hormones like cortisol (the stress hormone).[4]
In other words: depression affects the whole body, not just your thoughts.
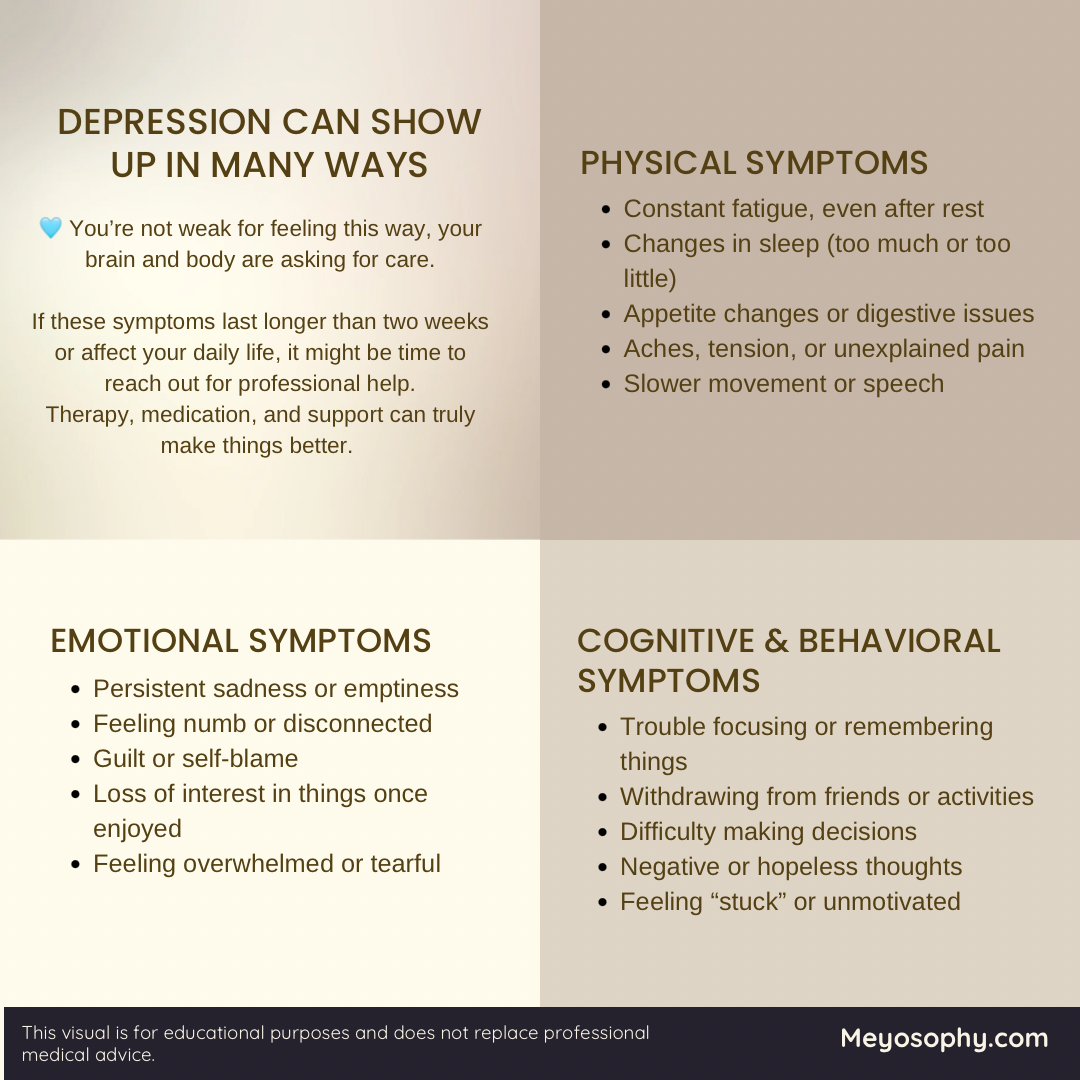
Common Symptoms (and How They Show Up in Daily Life)
Emotional symptoms:
- Persistent sadness, emptiness, or hopelessness
- Feeling worthless or guilty
- Loss of interest or pleasure in activities you once enjoyed
Physical symptoms:
- Fatigue or lack of energy
- Changes in sleep (too much or too little)
- Appetite changes (overeating or loss of appetite)
- Slowed movements or speech
Cognitive and behavioral symptoms:
- Difficulty concentrating or making decisions
- Withdrawing from friends and family
- Neglecting responsibilities
- Thoughts of death or suicide (if this happens, please reach out for help immediately, help is available 24/7 via hotlines listed below or your local emergency number).
Even small tasks (like showering, cooking, or replying to a message) can feel overwhelming when you’re depressed. It’s not laziness or weakness; it’s the illness making everything heavier.
What Causes Depression?
Depression has no single cause. It’s often the result of several factors coming together: biological, psychological, and social.
1. Genetics
If depression runs in your family, your risk is higher. Studies show that genetics account for about 40% of depression risk.[5]
2. Brain Chemistry
Imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine can affect mood and motivation.
3. Hormones
Hormonal changes (such as those during pregnancy, menopause, or thyroid problems) can trigger or worsen depression.
4. Stress and Trauma
Chronic stress, loss, or childhood trauma can rewire the brain’s stress response, making someone more vulnerable.
5. Lifestyle Factors
Lack of sleep, poor diet, little sunlight, and minimal physical activity can all contribute to or worsen depressive symptoms.
6. Medical Conditions
Chronic illnesses like diabetes, heart disease, and chronic pain are closely linked with higher rates of depression.[6]

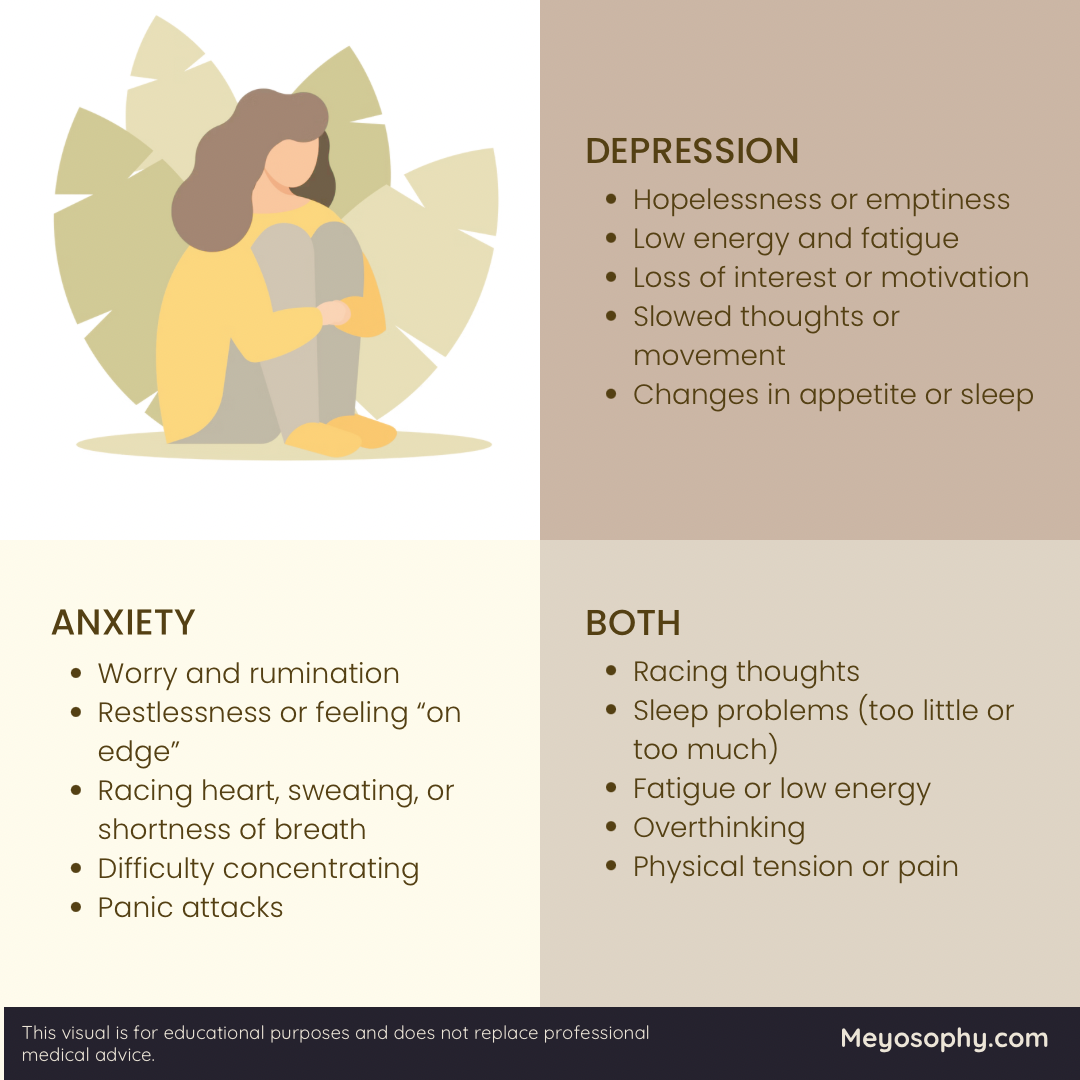
The Connection Between Depression and Anxiety
Depression and anxiety often show up together. About half of people with depression also have an anxiety disorder.[7]
Why? Because both conditions involve similar brain circuits related to stress, emotion, and worry. Anxiety tends to make the mind race; depression slows everything down. Together, they can trap someone in a painful loop of overthinking and exhaustion.
Treatment often helps both at the same time, especially when therapy and medication are combined.
Treatment and Recovery: What Helps
There’s no one-size-fits-all cure, but depression is treatable, often highly so. Most people recover fully or find ways to manage their symptoms.
1. Therapy
- Cognitive Behavioral Therapy (CBT): Helps reframe negative thinking patterns.
- Interpersonal Therapy (IPT): Focuses on relationships and communication.
- Mindfulness-Based Therapy: Combines meditation and self-awareness to reduce rumination.
Talking with a professional doesn’t mean you’re weak. It means you’re taking your mental health seriously, like you should.
Read more about different therapies for depression here.
2. Medication
Antidepressants like SSRIs (Selective Serotonin Reuptake Inhibitors) can help balance brain chemistry. They don’t make you “happy” overnight, but they can lift the fog enough for therapy and daily coping to work better.
Always consult a doctor before starting or stopping medication.
3. Lifestyle Support
Small steps matter. Regular movement (even short walks), eating nutritious foods, and maintaining a consistent sleep schedule all help regulate mood.
Studies show that exercise can be as effective as medication for mild to moderate depression in some cases.[8]
4. Social Connection
Depression often makes you want to isolate, but staying connected (even in small ways) is healing. Send a message. Sit with a loved one. Share silence. You don’t have to put a mask on. Just being together with someone in a room can help.
Real-Life Steps That Make a Difference
Recovery is rarely linear. Some days you’ll feel progress, other days you’ll slide back (and that’s okay).
Here are a few habits that can support you:
- Keep a simple daily routine (structure helps your brain feel safe).
- Get morning light exposure, it regulates your circadian rhythm.
- Write down small wins each day. A positivity- or gratitude journal may work well for you.
- Practice self-compassion. Healing isn’t instant.
If you’ve lived with depression for a long time, know this: your brain can change. New habits, therapy, and time can help rebuild the pathways that once felt blocked.

When to Reach Out for Help
If you’re feeling hopeless, overwhelmed, or having thoughts of suicide, please reach out right now. You are not alone, and help is available 24/7.
In the U.S.:
• Call or text 988 to reach the Suicide and Crisis Lifeline (available 24/7, free, and confidential).
• You can also chat online at 988lifeline.org.
Outside the U.S.:
• Visit https://findahelpline.com to locate international hotlines in your country.
If your depression is making it hard to function, sleep, or eat; or if these feelings have lasted for more than two weeks, it’s time to talk with a mental health professional.
Getting help early can make recovery easier and more effective. 💙
You Can Get Better
Depression can feel like a heavy, endless fog, but it is possible to find light again. Healing doesn’t mean you’ll never have a bad day; it means you’ll know how to move through it, one step at a time. Also, having a bad day once in a while is much better than depression everyday.
You are not broken. You are healing, even on the days it doesn’t feel like it. Try to take small steps and seek help if you can. Things can get better 💙
Sources
- World Health Organization. (2023). Depression: Key facts.
- Harvard Health Publishing. (2021). What happens in the brain during depression?
- Sheline, Y. I. et al. (2003). Increased amygdala response and reduced hippocampal volume in depression.
- National Institute of Mental Health. (2022). Depression and the Brain.
- Sullivan, P. F. et al. (2000). Genetic epidemiology of major depression: review and meta-analysis.
- World Health Organization. (2020). Depression and other common mental disorders: global health estimates.
- Kessler, R. C. et al. (2003). The epidemiology of major depressive disorder and comorbid conditions.
- Cooney, G. M. et al. (2013). Exercise for depression. Cochrane Database of Systematic Reviews.

