Sleep isn’t optional self-care, it’s a biological necessity. It affects your mood, your ability to manage stress, how well you remember things, and even how your brain processes emotions. If you want to feel calmer, think more clearly, and reduce the risk of mood problems, improving sleep is one of the most powerful tools you have.
This article explains, what sleep does for your mind, what happens when it’s poor, and practical steps you can take to sleep better.
Disclaimer: This article is for informational and educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your doctor, therapist, or another qualified health professional with any questions you may have regarding your physical or mental health, sleep problems, or any medical condition. Never disregard or delay seeking professional help because of something you have read here. If you experience ongoing insomnia, severe fatigue, or symptoms of a sleep or mental health disorder, please contact a healthcare provider or sleep specialist for assessment and support. Read our full disclaimer here.
Why sleep matters for your mental health
When you sleep well, your brain:
- Sorts and stores memories (including emotional memories).
- Processes emotions, helping you respond more calm the next day.
- Resets mood systems and balances stress hormones.
When sleep is poor or missing, those systems don’t work great. You get more reactive, less able to regulate emotions, and at higher risk for depression, anxiety, and other problems. There’s strong evidence that improving sleep improves mental health outcomes, not just the other way around.[1][2]

The numbers
Research shows that around one in three adults experiences symptoms of insomnia at some point. Things like lying awake for hours, waking up often, or feeling unrefreshed in the morning even after sleeping.
About one in ten people has a more serious, long-term sleep disorder that interferes with daily life. In the United States alone, it’s estimated that 50 to 70 million people live with some form of sleep disorder.
And that’s just what’s been diagnosed. Many more people quietly deal with poor sleep but never talk about it or get help for it. [3-7]
Common sleep issues
Sleep problems come in many forms, and not all of them look like the classic “I can’t fall asleep.”
- Insomnia – This is the most common issue. It can mean trouble falling asleep, waking up too early, or feeling like your sleep isn’t deep or restorative. When it lasts for months and starts affecting your mood or energy, it’s called chronic insomnia.
- Sleep apnea – In this condition, breathing repeatedly stops or becomes very shallow during the night. People often snore loudly, wake up gasping, or feel exhausted even after a full night’s sleep.
- Restless legs syndrome (RLS) – This causes an uncomfortable urge to move your legs, especially when you’re resting or trying to fall asleep. It can make it almost impossible to relax.
- Parasomnias – These include things like sleepwalking, sleep talking, night terrors, or sleep paralysis, unusual events that happen while you’re asleep or between sleep and wakefulness.
- Circadian rhythm problems – Sometimes your body clock just doesn’t line up with your daily schedule. You might not feel sleepy until very late at night (delayed sleep phase), or you might work shifts that constantly disrupt your rhythm.
- Excessive sleepiness or hypersomnia – Some people feel extremely tired no matter how much sleep they get. This can be related to underlying health or neurological conditions. [3-7]
The basics: how sleep is organized
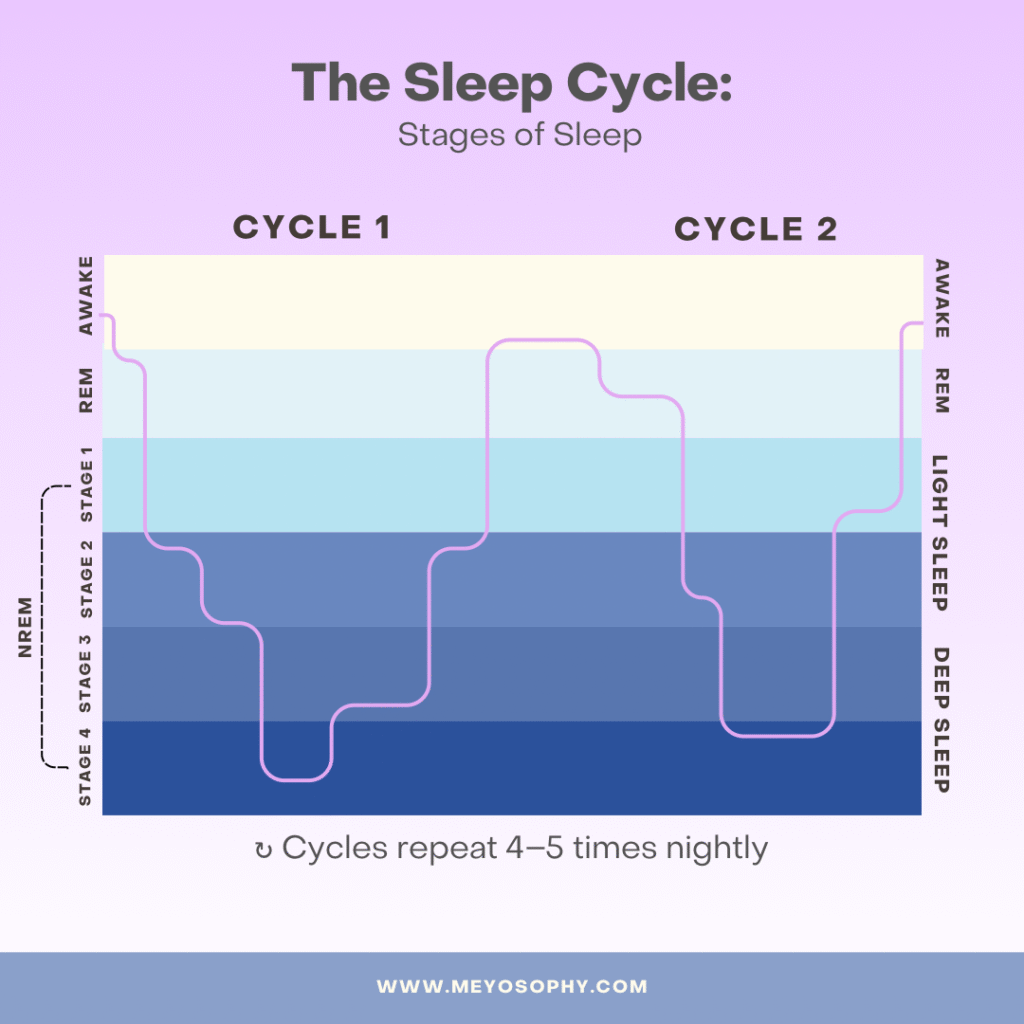
Sleep isn’t one single thing. Night sleep cycles through different stages roughly every 90 minutes:
- NREM (non-REM) sleep: includes light sleep and slow-wave (deep) sleep. Deep sleep is linked with physical recovery and some types of memory consolidation.
- REM (rapid eye movement) sleep: the phase where dreaming is most likely. REM is strongly linked to emotional processing and helping the brain “file” emotional experiences in a less raw, reactive form.
Both NREM and REM are important. Think of them as different parts of a nightly workshop where your brain repairs, organizes, and calibrates emotional responses for the next day.[10][13]
How sleep and mood link together: what the science shows
Three big ways sleep supports mental health:
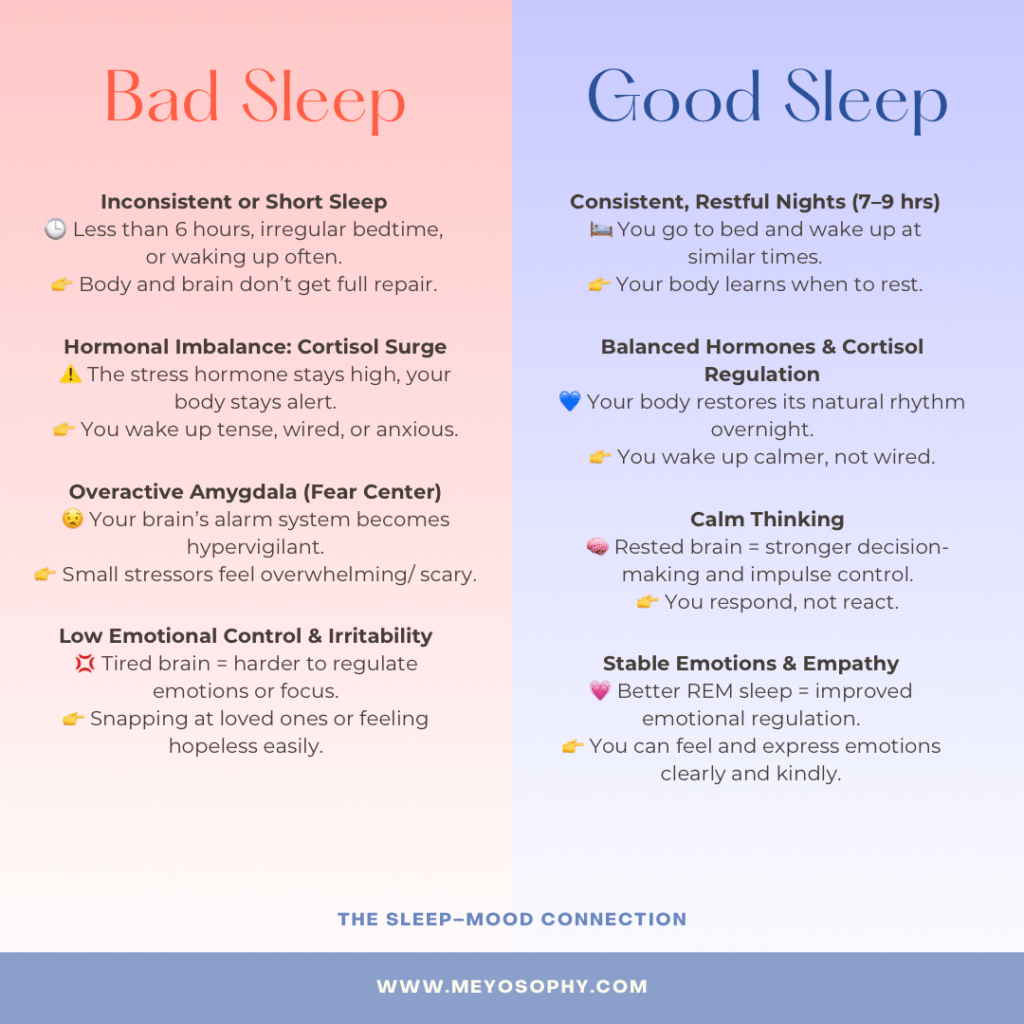
1. Emotional regulation (sleep helps you calm down).
Sleep, especially REM and the interplay between sleep stages, helps the brain process the day’s emotional events, reducing their intensity so you don’t wake up more distressed than when you went to bed. When you miss sleep, your amygdala (the brain’s alarm center) becomes more reactive, so small stresses feel much bigger the next day.[10][16]
2. Memory and learning (sleep helps you learn from experience).
Sleep consolidates memories. That includes emotional memories. Sleep helps keep the facts intact while softening the raw emotional charge. Without sleep, this balancing process weakens, and negative memories or biases can stick more strongly.[19]
3. Hormones & stress systems (sleep keeps the stress response in check).
Poor sleep raises baseline levels of stress chemicals (like cortisol and norepinephrine) and reduces the brain’s ability to bounce back from alarm signals. Over time this keeps you in a higher state of nervous system arousal: exactly what mood and anxiety disorders feed on.[2][9]
Poor sleep can cause or worsen mental health problems
Research shows that chronic insomnia or repeated short sleep increases the risk of developing mood disorders. People with chronic insomnia are more likely to develop depression and anxiety, and treating insomnia reduces the severity of those conditions in many trials.[11][12]
This is why clinicians often treat sleep problems as a first-line target: get sleep on track and mood/immunity, and stress responses often improve too.
Mental health disorders tied to sleep disruption
Poor sleep doesn’t just feel bad: it’s a risk factor and reinforcing factor in many psychiatric conditions. Here are key links:
1. Depression
- Insomnia and short sleep duration frequently precede clinical depression.
- Sleep disruption worsens mood symptoms, suicidal ideation, and impairs the response to antidepressants.
- In studies, treating insomnia often reduces depressive symptoms, sometimes even when depression treatment is kept constant.
2. Anxiety and Generalized Anxiety Disorder (GAD)
- Anxiety frequently leads to sleep onset problems (worrying, racing thoughts).
- Poor sleep creates a feedback loop where anxiety gets worse, which then further disrupts sleep.
3. Bipolar Disorder
- Sleep disturbances (especially reduced need for sleep) can tip someone into manic or hypomanic episodes.
- Stabilizing sleep is a core part of managing mood swings in bipolar disorder.
4. Post-Traumatic Stress Disorder (PTSD)
- Nightmares, fragmented REM sleep, and hyperarousal often interfere with restorative sleep.
- Poor sleep impairs emotional memory processing and heightens emotional reactivity, both central to PTSD symptoms.

5. Substance Use & Addiction
- Many substances disrupt sleep (cocaine, stimulants, alcohol) or cause rebound insomnia during withdrawal.
- Poor sleep can increase cravings and relapse risk.
6. ADHD and Cognitive Disorders
- Sleep problems impair attention, executive function, and working memory. Important symptoms for people with ADHD.
- In individuals with ADHD, untreated sleep issues often worsen symptoms.
What actually improves in mental health when sleep gets better?
When sleep quality improves you can expect:
- Better mood stability and less irritability.
- Lower anxiety and fewer panic-like reactions.
- Improved concentration and memory.
- Better emotional recovery after stressful events.
Randomized trials and meta-analyses show that sleep treatments, especially cognitive behavioral therapy for insomnia (CBT-I), lead to reductions in depressive and anxiety symptoms, and these benefits often last.[12][20]
Practical strategies: what actually helps
You don’t need a lab to start improving sleep. Here are practical, research-backed strategies:
1. Aim for quality and quantity
Most healthy adults do best with about 7–9 hours of sleep per night; for many people, 7+ hours is the minimum to support brain and mood health.[9] So, make sure you get enough time in bed.
2. Keep a consistent schedule
Go to bed and wake up at (roughly) the same time every day. Yes, even weekends. Regular timing strengthens your circadian rhythm, making sleep easier and deeper. It gets you into a rhythm.
3. Create a wind-down routine
Do 30–60 minutes of calming activities (read, stretch, warm shower) and avoid screens or work right before bed. Light from screens interferes with melatonin, the sleep hormone.
4. Build a sleep-friendly bedroom
Make your place of sleep: cool, dark, quiet, and comfortable. Reserve the bed mostly for sleep and sex (not work or doom-scrolling).
5. Watch stimulants and alcohol
Caffeine late in the day and alcohol near bedtime both fragment sleep. Alcohol can make you fall asleep fast but reduces REM and deep sleep later in the night.
6. Move your body (but time it right)
Regular physical activity improves sleep quality, but intense exercise right before bed can be activating for some people. So move your body earlier in the day.
7. Try CBT-I if insomnia is persistent
If you struggle to fall asleep or stay asleep regularly, Cognitive Behavioral Therapy for Insomnia (CBT-I) is the first-line, evidence-based treatment and often helps more than sleeping pills in the long run.[12][20]
8. Treat medical sleep disorders
If you snore loudly, stop breathing during sleep, or are extremely sleepy during the day, ask your doctor about obstructive sleep apnea (OSA). Treating OSA (for example with CPAP) often improves mood and cognition.
What about sleep apps and short fixes?
Sleep apps (guided meditations, sleep sounds, relaxation audios) can be useful short-term tools, especially for building routine. But for chronic insomnia or severe sleep disruption, structured CBT-I (with a therapist or a validated digital CBT-I program) is more effective than general apps or pills.[12]
A realistic plan to improve sleep this month
If you want a practical 4-week plan:
First week: Baseline & habit: Track sleep times and awakenings. Choose a fixed wake time. When do you want to be asleep?
Second week: Wind-down & environment: Build a 30–60 minute bedtime routine and optimize the bedroom.
Third week: Limits & caffeine: Move afternoon caffeine earlier, avoid alcohol near bedtime, and do light exercise earlier in the day.
Fourth week: Evaluate & escalate: If things improved, keep going. If insomnia persists (trouble falling asleep >3 nights/week for weeks), book an appointment for CBT-I or a sleep clinic referral.
When to see a professional
Talk to your GP or a sleep specialist if:
- You’re struggling with sleep most nights for more than a month despite good habits.
- You fall asleep unintentionally (nodding off) during the day.
- You or a partner notice breathing pauses or very loud snoring.
- Your sleep problems are making depression, anxiety, or day-to-day functioning worse.
CBT-I providers, sleep medicine clinics, and even some trained psychologists can help with insomnia; primary care can rule out medical causes and refer you for further testing (e.g. for sleep apnea).
Final thoughts: sleep is a low-cost, high-impact treatment
Improving sleep is one of the most practical ways to support mental health. It’s not a fix all solution: therapy, medication, social support, and medical care all have their places, but sleep is a foundation. Better sleep makes everything else (mood, focus, resilience) easier to manage. Start small: consistent wake times, a calming wind-down, and an honest look at late-day caffeine can go a long way. If insomnia is persistent, CBT-I is the evidence-backed next step.
Sleep well, and your mind will thank you for it.
Sources & further reading
- Scott, A.J., Webb, T.L., Hames, S., et al. Improving sleep quality leads to better mental health: a meta-analysis and causal modelling study. Sleep Medicine Reviews / PubMed Central (2021). https://pubmed.ncbi.nlm.nih.gov/34607184/
- NHLBI / NIH. Sleep Deprivation and Deficiency: How Sleep Affects Your Health. National Heart, Lung, and Blood Institute. (2022). https://www.nhlbi.nih.gov/health/sleep-deprivation/health-effects
- American Academy of Sleep Medicine, “Sleep Disorders and Statistics,” 2024.
- National Institutes of Health, “Epidemiology of Insomnia,” 2023.
- Sleep Foundation, “How Many People Struggle with Sleep?,” 2024.
- Centers for Disease Control and Prevention (CDC), “Short Sleep Duration Among Adults,” 2024.
- National Center for Biotechnology Information (NCBI), “Prevalence and Impact of Sleep Disorders,” 2023.
- CDC. Sleep Facts & Stats. Centers for Disease Control and Prevention (2024). https://www.cdc.gov/sleep/data-research/facts-stats/index.html
- Harvard Health Publishing. How sleep deprivation can harm your health. Harvard Health (2025 update). https://www.health.harvard.edu/staying-healthy/how-sleep-deprivation-can-harm-your-health
- Goldstein, A.N., Walker, M.P. The Role of Sleep in Emotional Brain Function. Annual Review / Walker Lab (2014). https://walkerlab.berkeley.edu/reprints/Walker_NYAS_2009.pdf
- Clement-Carbonell, V., et al. Sleep Quality, Mental and Physical Health: A Differential Relationship. Frontiers / PMC (2021). https://pubmed.ncbi.nlm.nih.gov/33329588/
- Furukawa, Y., et al. Review Article: Cognitive Behavioral Therapy for Insomnia (CBT-I) effectiveness. Journal of Affective Disorders / Sleep Research reviews (2024). https://doi.org/10.1111/jsr.70058
- Sleep Foundation. REM Sleep: What It Is and Why It’s Important. (2025). https://www.sleepfoundation.org/stages-of-sleep/rem-sleep
- Consensus Panel. Recommended Amount of Sleep for a Healthy Adult: Joint Consensus Statement (AASM & SRS). Journal of Clinical Sleep Medicine (2015). https://pmc.ncbi.nlm.nih.gov/articles/PMC4513271/
- Blackwelder, A., et al. Effect of Inadequate Sleep on Frequent Mental Distress. Preventing Chronic Disease (2021). https://www.cdc.gov/pcd/issues/2021/20_0573.htm
- Rawson, G., et al. Sleep and Emotional Memory: recent reviews. Sleep & Emotion literature (2024). https://link.springer.com/article/10.1007/s40675-024-00306-8
- Shin, J.W., et al. Improving mental health and daytime function in adult insomnia: CBT-I outcomes. PMC (2023). https://pubmed.ncbi.nlm.nih.gov/36964212/
- Mayo Clinic. Depression, anxiety and sleep: How are they linked? (overview and tips). https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/sleep/art-20048379
- Payne, J.D., et al. Sleep promotes lasting changes in selective memory for emotional scenes. Frontiers in Integrative Neuroscience (2012). https://www.frontiersin.org/articles/10.3389/fnint.2012.00108/full
- Ntikoudi, A., et al. The Effectiveness of Cognitive Behavioural Therapy on Sleep Quality (CBT-I) in Women: 2024 Review. PMC (2024). https://pubmed.ncbi.nlm.nih.gov/ (see journal)

